IC-CS Risk Study
IC-CS Risk Study Goals & Metrics
The IC-CS Risk Study aims to address critical disparities in maternal health outcomes by testing the effectiveness of the IC-CS Risk Calculator in labor units across the United States. With over four million births annually and cesarean deliveries linked to increased maternal morbidity, this study focuses on reducing unnecessary cesareans, particularly among birthing people undergoing labor induction. The study's central goal is to assess whether the calculator, which provides individualized cesarean risk predictions, can improve clinical decision-making, reduce cesarean rates, and mitigate racial disparities in obstetric outcomes.
Using a randomized stepped-wedge rollout design across 14 labor units, the study will:
- Evaluate site-specific factors to develop tailored implementation strategies.
- Measure the effectiveness of the calculator in reducing cesarean deliveries, with a focus on its impact on racial disparities.
- Assess the tool's acceptability, usage, and equitable reach through a mixed-methods approach.
By the study's conclusion, the research team will provide actionable insights on the calculator's impact, alongside an online toolkit for broad implementation, offering a pathway to improved maternal health outcomes nationwide.
Implementation of Calculated Cesarean Section Risk (IC-CS Risk)
The IC-CS Risk initiative is a groundbreaking, multi-site project designed to implement a cesarean risk calculator that provides clinicians and patients with individualized cesarean risk percentages during labor induction.
With a focus on reducing cesarean deliveries, improving maternal health outcomes, and addressing disparities affecting Black, Indigenous, and People of Color (BIPOC) birthing individuals, this project spans six major health systems, including:
- Cleveland Clinic
- Henry Ford
- University of Pennsylvania
- University of Michigan
- Intermountain Health
- University of Utah.
Over three years, the calculator will be systematically introduced across 14 labor and delivery units, allowing for strategic evaluation and measurable improvements in maternal care.
How will IC-CS measure impact?
- Clinical Outcomes: Tracking changes in maternal morbidity and cesarean section rates to evaluate the effectiveness of the calculator in improving labor outcomes.
- Utilization: Assessing how frequently the calculator is used across different labor and delivery units to ensure widespread adoption.
- Equity: Evaluating whether the calculator reaches all target patients, with a focus on race, ethnicity, and insurance status, to ensure equitable access and outcomes.
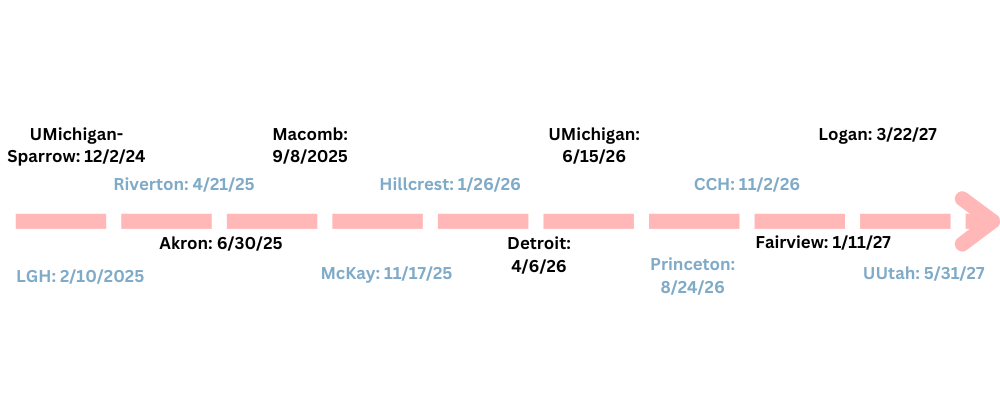
Timeline of Implementation
Meet The Team
 Rebecca F. Hamm, MD MSCE
Rebecca F. Hamm, MD MSCE
 Meghan Lane-Fall, MD, MSHP
Meghan Lane-Fall, MD, MSHP
 Lisa Levine, MD, MSCE
Lisa Levine, MD, MSCE
 Mucio Kit Delgado, MD, MS
Mucio Kit Delgado, MD, MS
 Rebecca Clark, MSN, PhD
Rebecca Clark, MSN, PhD
 Elizabeth Howell, MD, MPP
Elizabeth Howell, MD, MPP
 Alisa Stephens, PhD
Alisa Stephens, PhD
 Michelle Moniz, MD, MSc
Michelle Moniz, MD, MSc
 Brett Einerson, MD, MPH
Brett Einerson, MD, MPH
 Jessica Page, MD, MS
Jessica Page, MD, MS
 Meaghan McCabe, MPH
Meaghan McCabe, MPH
 Sarah Hulse
Sarah Hulse